Medical Research Society advances UT science
Targeted molecules may one day treat disease without side effects
By Laurie B. Davis

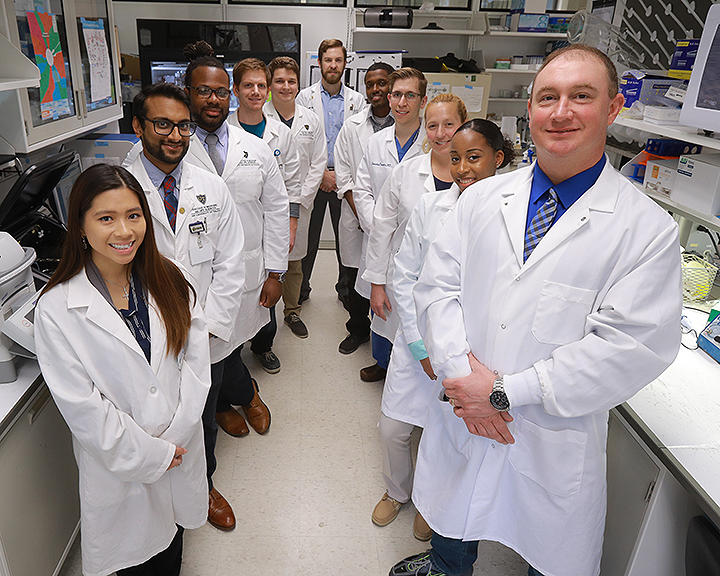
Dr. Terry Hinds (PhD ’10), assistant professor of physiology and pharmacology and of urology, has developed two new molecular drugs, Thin molecules and Sweet-P, for which he has patents.
Thin molecules may lead to new medications that reduce blood glucose levels for Type-2 diabetics, while also preventing weight gain and high blood pressure that can cause cardiovascular disease. Sweet-P is an anti-cancer molecule that binds directly to DNA and inhibits the growth of cancer cells. These novel drugs need to first be tested in mice before testing in humans can be done.
Hinds’ research projects are promising and could receive funding from the National Institutes of Health within one year. These factors made him a prime candidate for receiving seed money from The University of Toledo Medical Research Society to further investigate and move his research projects forward.
The University of Toledo Medical Research Society comprises philanthropists in the Toledo community who have come together to create a permanent endowed source of seed funding for young researchers in The University of Toledo’s College of Medicine and Life Sciences. Society members focus on providing funds to advance innovative biomedical research projects that will benefit the Toledo community and well beyond Northwest Ohio.
Since 2015, the society has granted awards of $50,000 to four UT scientists in the COMLS. The Society supports qualified faculty members in the early stages of their careers, such as assistant and associate professors, like Hinds.
In 2015, the Society supported the research of Dr. Katheryn Eisenmann, assistant professor of biochemistry, for her research to develop a drug to fight ovarian cancer. In 2016, Dr. Joshua Park, assistant professor of neurosciences, received $50,000 from the Society to continue his study on Alzheimer’s disease and seek a pharmaceutical company to assist in further testing. The third $50,000 grant was given to Dr. Steven T. Haller, assistant professor of cardiovascular medicine, to advance his research in the development of a novel therapy for the treatment of kidney disease. Hinds is the 2018 recipient of $50,000 from the Society.
Typically, the Society financially supports those who have proven the worthiness of their research to the NIH or other national funding agencies and have received positive reviews. Like Hinds’ work, the project requires additional, preliminary data or proof-of-concept studies to garner much larger grants the NIH can offer. So far, the investment from members of the Medical Research Society already has generated nearly $1 million in external research funding for the College of Medicine and Life Sciences.
The Society’s contributions are vital resources that continue to advance science at UT. “The Medical Research Society is a wonderful way to invest in research and be an active participant in philanthropy,” says Dr. Christopher Cooper, executive vice president for clinical affairs and dean of the College of Medicine and Life Sciences. “We are very excited about the work that is being done by the research grant recipients and grateful to those who have invested in them. We are looking forward to growing our membership to the society,” says Cooper.
‘GRbeta is my baby’
To understand how Hinds and his research team got to the point they are now, his earlier studies and findings can highlight how he came to develop the molecules that may be used for human drug therapies. Already there is interest from companies in the Sweet-P technology. It all relates to two nuclear receptors called GRalpha and GRbeta.
When Hinds first joined UT in 2005, he was working with Dr. Edwin Sanchez studying glucocorticoids, which are stress hormones such as cortisol, and looking at how these could be regulating different states of obesity. It was known then that cortisol could cause significant weight gain in people because of long-term stress or long-term therapy. But Hinds notes that short-term cortisol is triggered by a process that breaks down fat: the sympathetic nervous response, better known as the “fight or flight” response. “So, there’s a conundrum that exists,” says Hinds.
This disparity made Hinds dig deeper into understanding GRbeta. The sequence of the GR gene was discovered in humans in 1985, and revealed two major isoforms from one gene, a GRalpha and GRbeta. However, a paper published in 1997, in a high impact journal by a group of German researchers, reported that mice did not express GRbeta.
“At the time, there was the glucocorticoid receptor GRalpha, that’s the receptor that binds cortisol,” says Hinds, “and I realized that there might be another receptor, and I started looking for it even though it was against the dogma. We found that mice do have GRbeta, but in a different location on the GR gene compared to humans, and like human GRbeta, it couldn’t bind cortisol and causes glucocorticoid resistance. Your body at first makes you lean, from cortisol/glucocorticoid treatment because it’s binding to the alpha, and then when you have long-term stress, it increases the beta and you become resistant to glucocorticoids like with Type-2 diabetes when someone becomes insulin-resistant.”
Hinds published the discovery of murine GRbeta in 2010. GRalpha controls metabolism, immunity and other physiological processes, and GRbeta inhibits GRalpha, producing a state of glucocorticoid resistance. His breakthrough research in finding GRbeta in mice would now make it possible to study its effects on human physiology and disease. “Now, we can use mouse models to determine the effects of the alpha and beta on obesity and diabetes,” says Hinds.
As the American diet has changed over the past 50 years, more and more Americans are overweight, obese or severely obese. Hinds says it’s because the food serving is four times the size it once was. “And a lot of that has to do with the soda. I mean the burgers are bigger, but the amount of sugars that we’re taking in is a lot,” he says.
Hinds says that in the 1960s, about 10 percent of the population was obese. By 2030, he says, it’s predicted that 50 percent of the population will be severely obese; overall, 90 percent of the population will be obese or overweight. “One of the things I look at is the liver. We look at the alpha and the beta. When you eat a big fat diet, you get a fatty liver. You can have insulin resistance and not necessarily have a fatty liver. But if you have a fatty liver, you’re probably going to have insulin-resistant diabetes,” says Hinds.
Gene editing
The UT Medical Research Society grant allowed Hinds and his team to accomplish a genetic feat: making a mouse with only the GRalpha expressed by removing the GRbeta, a difficult task because the two isoforms are located on the same gene.
Hinds had submitted some of the team’s research on GRbeta to the NIH before receiving the Medical Research Society grant. But before they could get the $2 million NIH grant, they had to answer some additional questions about their mice such as what is their phenotype — are they obese, diabetic, do they have fatty liver? “We put on our grant that we could possibly make the gene-targeting technology called CRISPR precisely cut out the beta and not the alpha, but we weren’t sure because there’s only one gene. They wanted to see if we could do that,” says Hinds.
Having heard a speaker at UT, who presented on CRISPR (Clustered Regularly Interspaced Short Palindromic Repeats), a new gene-targeting technology, Hinds connected with her. He worked with Dr. Shondra Pruitt-Miller of St. Jude Children’s Hospital in Memphis. Pruitt-Miller’s expertise with CRISPR and her collaboration with Hinds brought the Hinds lab the tool that could genetically edit out the GRbeta and retain the GRalpha. “Before this technology, there was no way to make a mouse that had just alpha or just beta. We’ve been working on this for several years, and the technology was only available within the last couple of years,” he says.
Funding is fundamental
The Medical Research Society grant came at just the right time for Hinds because earlier funding he’d received was drying up. “We’re trying to get money, so we can really try and understand what’s medically and scientifically going on,” says Hinds. “Without this type of funding, we don’t keep our projects moving, and right now there’s a huge gap, and if I didn’t get the money, I wouldn’t be able to keep things moving, I wouldn’t be able to get the knock-out mouse or the CRISPR technology.” Progress, he says, would be stalled and momentum lost.
The Society’s support is extremely impactful for the medical school, says Hinds. “It benefits the medical school because new students get to work with researchers and get published for doing this research, and that gets them better residencies. When the MRS invests in researchers who get the (NIH) funding, it’s a reinvestment back into the medical school,” he adds.
Hinds is excited about Sweet-P’s potential as a treatment for cancer, as well as other diseases. “It actually goes in and binds to the human GRbeta gene and stops it from being expressed. It’s the only drug like it. Now we realize we can design many other drugs in a similar fashion for a lot of other targets,” says Hinds.
“Your typical drug pathways, like the mechanisms and actions I teach for the medical school is that you have something that binds and sticks to a protein that stops or enhances the protein function. It’s how aspirin and every other drug currently work; well this one doesn’t do that. It binds to the DNA and inhibits right at the gene.”
Hinds says this novel drug also will reduce side effects because of its precision. “It’s one target, one concept.”
For more information about the Medical Research Society and becoming a member, please contact Jodi Farschman at 419.530.2646 or jodi.farschman@utoledo.edu.